Designing a sustainable hospital fit for an uncertain future
As part of our series of articles looking at Buro Happold’s Hospital of the Future project, we examine how future hospitals will need to consider low carbon as well as more resilient supply chain solutions.
We are already exceeding the consumption boundaries of a healthy planet. Step forward twenty years, and all construction projects will need to consider not just mitigation to lessen the impact on climate change, but critically also adaptation to live with climate change.

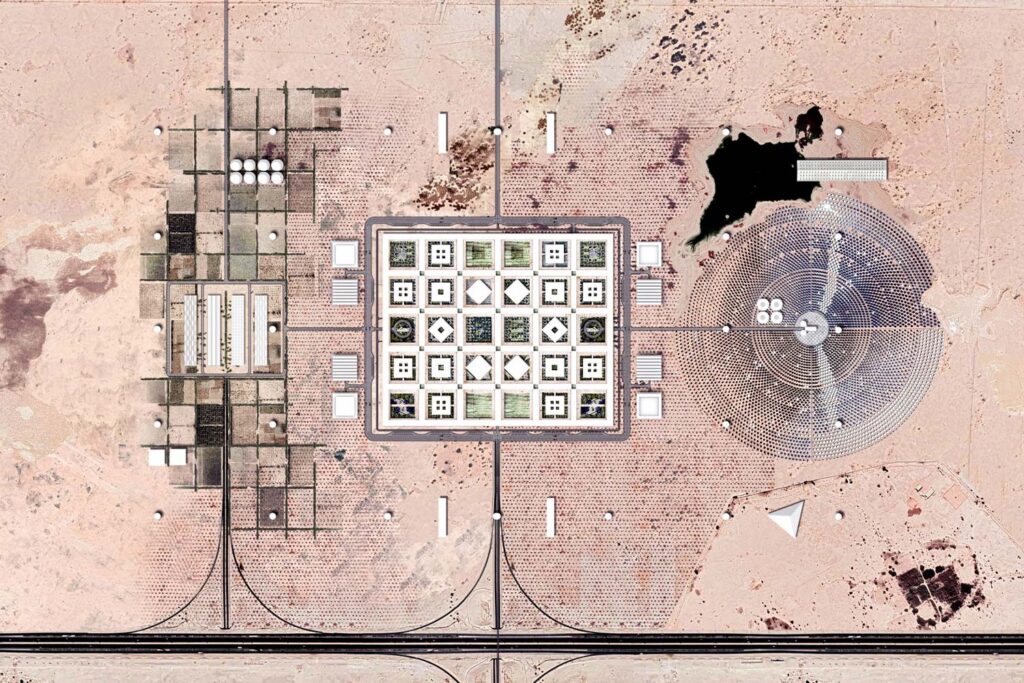
New hospitals in the future will be no exception. As part of its ground-breaking conceptual Hospital of the Future project, Buro Happold has worked alongside OMA and other collaborators after being commissioned to explore how hospital design could be reimagined to be more adaptable to a changing world.
Our multidisciplinary team of experts re-examined hospitals from the first principles of design, to develop a prototype for effective and efficient future hospitals. In our previous article, we examined how the prototype envisions agile modular horizontal structures, located in out-of-town locations, which ensure for clients that their hospital never becomes obsolete.
Our research also identified the importance of “treading the Earth lightly” and building resilience against future shocks, stresses and supply chain vulnerabilities.
Using renewables to power hospitals
The prototype is less constrained than the typical inner-city hospital of today. This affords the opportunity to incorporate infrastructure that reduces vulnerability through increasing site self-sufficiency.
Situated within a desert environment, solar energy will be in abundance for the prototype. The horizontal plane creates significant roof space for the integration of solar photovoltaics (PVs). When other plant is accounted for, 380,000m2 of PV could be installed at roof level meeting 35% of the prototype’s energy demand. Additional PV modules could also be incorporated within the land around the prototype, given its out of town nature and lower land values. An additional 520,000m2 would be required to meet all hospital annual demands.

A Battery Energy Storage System (BESS) and Thermal Energy Storage (TES) could be deployed to balance demands between day and night. A smart grid architecture would manage and operate all the energy assets within the site and maximise the renewable energy utilisation as well as the overall efficiency.
The concept allows the design to evolve flexibly to make best use of the natural assets local to the hospital site – so for sites further away from the equator, the design could need to be balanced more towards a heavier reliance on other forms of renewables.
The generation of energy using hydrogen enables seasonal storage to maximise renewables generation and guarantee 100% green power supply during the peak summer months. It also has a critical by-product – oxygen, which could potentially be used within the hospital’s systems.
Reducing the carbon emissions of the prototype is key, in line with the climate action agenda. However, given that this energy can be delivered in a low or zero carbon way, this enables trade-offs to be addressed when considering demand reductions for other vital and finite resources, such as water.
Tackling water demands
A typical present-day hospital in an arid environment has three main water demands: district cooling, hospital water use, and irrigation. Typically, district cooling water makes up 47% of total hospital water demand, while hospital water use is 36% and irrigation demand is 17%. In the development of the prototype, four key areas of study were identified to reduce water demands: efficient district cooling, internal fixtures, fittings and user behaviours, water recycling and reuse, and sustainable irrigation strategies.
Through interventions in these areas, it is believed the prototype can reduce demands from a typical baseline of 11,800m3 per day (based on today’s equivalency to the prototype) to 3,300m3 per day, resulting in a 72% reduction – an enormous operating benefit for the end client.

However, if a xeriscaping (planting using drought-resilient species) was implemented, demands could be reduced to 2,600m3 per day, resulting in a 78% reduction. While the proposed solution does not provide a completely self-sufficient water system, significant improvements are made over the hospital of today.
Of all the proposed methods of reducing water demand, water recycling is the most culturally challenging. In a growing number of places, drinking highly treated municipal wastewater, called ‘reused water’, has become the best option — and, in some cases, the only one. But anxieties about reused water, often heightened by sensationalist media coverage, have prevented several projects from going ahead.
At least three important economic centres — Singapore, Windhoek in Namibia and Orange County in California — would not have progressed to where they are today without reused drinking water. Windhoek was the first city to create a drinking-water supply from reused water in 1968. The Goreangab Water Reclamation Plant currently produces around 24% of Windhoek’s drinking water.
NEWater supplies about 40% of Singapore’s drinkable and non-drinkable water. If all goes to plan, by 2060, it will meet 55% of the city’s water demands.
“If you look at the International Space Station, all resources get recycled continually, so it demonstrates it can be done,” says Buro Happold’s Neil Harvey, who provided infrastructure expertise to the project. “Perhaps we ought to be thinking more along these lines for our hospitals. It’s just about having the right mindset.”
Resilient supply chains
To increase resilience, the Hospital of the Future would be informed by a vulnerability assessment of key resources and supply chains on which the successful operation of the hospital is reliant. The assessment undertaken for the prototype considers national and regional resilience strategies. The outcomes of this – where it is believed vulnerabilities exist – then inform the spatial planning process.
In the prototype, this process identified that food, medical labour, drugs and pharmacy goods predominantly rely on international supply chains and skills. Such international supply chains may have high vulnerability to geopolitical shifts and tensions. As such, within the prototype, areas for onsite agriculture and pharma production have been specified.
To support the development of a prototype that is capable of riding out a significant shock or stress event, a critical function area has been tested based on its potential to operate self-sufficiently – as an island – over a series of time-based scenarios.
Harvey explains: “We developed this concept of an island mode of operation, which would allow you to operate in the event of being cut-off from certain supplies for a certain amount of time, to allow the hospital to continue to perform its critical functions.”
The outcomes of this assessment suggest that the hospital would be able to operate self-sufficiently for almost a week. At this point, the production of food to sustain the dietary requirements of staff and patients would become stressed, though there is still capacity within the energy water and waste systems. After one month, waste storage capacity of the hospital would be fully utilised.
The criticality of resilient supply chains was vividly demonstrated during the development of the Hospital of the Future project, as hospitals around the world faced life-threatening shortages in oxygen supplies for Covid-19 patients at the height of the pandemic.
“It brought home to everyone what the impact of these kinds of supply chain shortages could have in the coming years,” Harvey says.
Read more on the Hospital of the Future project: How to create a healing environment.